Dr. Taylor and the Robot
Only one surgeon in Iowa is trained to perform robotic-assisted lung surgery.
By Steve Sullivan
Dr. Mark Taylor is the only surgeon in Iowa doing robot-assisted lung surgery, including lobectomies. Taylor, who is with McFarland Clinic, performs surgery at Mary Greeley Medical Center. The hospital recently added a second da Vinci surgical robot. Robot-assisted surgery is a minimally invasive option that can result in less pain and faster healing for patients. Learn about Taylor’s work and meet two of his patients who have undergone robot-assisted lobectomies.
“The first thing I thought
when I met [Dr. Taylor] was
that he looks like an ex-NBA
player. Dr. Taylor did an
amazing job. I don’t think he
could have made a straighter
line where the lobe was.”
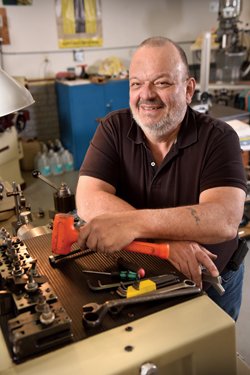
– JAMES ADAMS
James Adams was having a rough year. In late fall 2014, the Marshalltown man had a hip replacement. Not long after that, he experienced trouble urinating, which required surgery to remove a section of his prostate that was blocking urine flow. Then a chest x-ray indicated that a spot on his lung detected a few years earlier during a blood clot issue had grown. In early 2015, a biopsy indicated cancer. Adams would now need a lobectomy to remove the lower lobe of his left lung.
Adams’ oncologist, McFarland Clinic’s Dr. Debra Prow, immediately referred him to Dr. Mark Taylor, a McFarland surgeon who specializes in lung, or thoracic, surgery. “He’s the best in the area and he’s who you want doing this,” Prow told Adams.
The timing was fortunate. Taylor, who has more than two decades of experience, had recently completed training to do lobectomies with a surgical robot. In fact, he’s now the only surgeon in Iowa doing robot-assisted lung surgery, which can significantly reduce pain and recovery time for patients.
“The first thing I thought when I met him was that he looks like an ex-NBA player,” says Adams of the 6’ 7” Taylor. “He told me that he thought I would be an excellent candidate for robot-assisted surgery. He also told me that I would be his first robot-assisted lobectomy patient.”
Adams didn’t hesitate. A retired engineer with Fisher Controls, Adams had two friends who underwent successful robot-assisted prostate surgery. Adams had surgery in March 2015. It took six hours. The next day, he walked the hallway of Mary Greeley’s Intensive Cardiac Care Unit, and was home in less than a week. “I went back three months later for another chest x-ray and the technician couldn’t tell I’d had surgery,” he says. “I looked at the x-ray myself and you can’t tell except my lung looks small. Dr. Taylor did an amazing job. I don’t think he could have made a straighter line where the lobe was.”
Skeptic No More
Mary Greeley has had a robot-assisted surgery program since 2010, but Taylor, a highly respected general surgeon, had always been skeptical of the technology. Was it any more effective than other minimally invasive surgical methods? Did the cost of a surgical robot justify the benefits?
“I’ve worked in Guatemala doing a dozen hernia surgeries a day with equipment most people have in their basement shops,” says Taylor.
Taylor is no novice. He has performed more than 2,000 chest surgeries over the course of his career. Most are thoracoscopy, which is a minimally invasive procedure used for a variety of lung surgeries, such as wedge resections to remove a portion of a lung and diagnostic procedures, including collecting tissues for analysis by pathology. Thoracoscopy cannot be use for lobectomies, which typically involve opening up the chest. It’s a painful procedure that can require a week or longer hospital stay.
Taylor is not a risk taker so learning a new approach at this stage in his career – especially one that involved technology he questioned – was not likely.
At the same time, many of Taylor’s McFarland colleagues were steadfast proponents of robot-assisted surgery. So at the urging of a colleague, Taylor traveled to Ohio State University (OSU) to see Dr. Patrick Ross, another veteran surgeon, perform lobectomies with a surgical robot. It involved small incisions, which allowed for the insertion of necessary surgical instruments. Taylor also learned that robot-assisted lobectomy patients usually go home after just a few days in the hospital.
“It was a huge shock to me. A reality-bending trip,” admits Taylor. “I didn’t think you could do a lung lobectomy without getting into the chest. But I saw Ross do it and do a good job.”
After his OSU experience, Taylor felt a responsibility to embrace the potential for robot-assisted lung surgery.
“Chest surgery is painful. It involves opening a hard shell of chest wall and getting to vital organ within. You’re removing half the lung, along with major vessels that feed and drain it,” says Taylor. “I’ve done thousands of these procedures and have a solid base of positive outcomes. But I hate watching people hurt afterwards. My only motivator with learning to do this robotically is decreasing patient suffering, decreasing recovery time and decreasing the side effects of lung surgery.”
Training, Training, Training
Instead of a large incision in the side of the chest, robot-assisted surgery involves three small incisions in the chest through which a camera and surgical instruments are inserted. With the skilled assistance of surgical nurses, the surgeon properly positions the instruments and then utilizes a console in the corner of the operating room. There, the surgeon operates the instruments – cutting, cauterizing, suturing and moving organs as needed. The console provides high-def, 3D images from inside the patient’s body, which
are also broadcast on screens above the operating table.
Mary Greeley’s robot-assisted surgical program involves general surgery, including
hernia and gallbladder; urological surgery, including prostatectomies; and gynecological surgeries, including hysterectomies. To that, Taylor has introduced robot-assisted thoracic surgery. It is particularly complex because the lungs are so close to the heart, requiring
delicate maneuvers around vital arteries.
After his return from OSU, Taylor spent a year on an odyssey of robotic surgery discovery, education and training. He traveled to major cities, observing other surgeons. “This fuses what I’m already doing in thoracoscopy and open chest surgery,” he says. “The robot has more potential though. It gives you little hands with 549 degrees of axis. I’m able to put little hands under my control into the chest. My moves are small and more precise.”
A robot-assisted lobectomy, Taylor notes, takes almost twice as long as open chest surgery. But the trade-off is worth it, Taylor says, thanks to the reduced pain for the patient. Because of this, Taylor, with patient-approval, now performs all of his lung procedures with the robot. He has done more than a dozen lobectomies and 60 other lung procedures.
“Every person I’ve recommended it to has said ‘Yes.’ Not a single person wants the surgery the old fashioned way,” he says.

Robotic Advances in Thoracic Surgery
A presentation on robot-assisted lung surgery by Dr. Mark Taylor. Dr. Taylor explains how he uses a surgical robot for this type of surgery and shares some videos of surgeries.
Learn more about Robot-Assisted Surgery.
A Nagging Cough

“Dr. Taylor drew it all out for me –
‘This is what we have going on
and this is what we’ve got to
do to get that out of you.’
He told me we could do it robotically.
He put me totally at ease, and
I was scheduled for surgery in
less than a week.”
– MARCIA ANDERSON
Marcia Anderson was one of those who said “Yes.”
In September 2014, Anderson played with a surgical robot at an event sponsored by Mary Greeley at Iowa State’s Jack Trice Stadium. Little did she know at the time, but she would soon experience robot-assisted surgery personally.
In May 2015, Anderson had a persistent cough due to pneumonia. Antibiotics failed to completely clear up the lingering condition. Dr. Ricardo Arbulu, McFarland Clinic infectious disease specialist, suggested waiting a few months to see if the condition cleared up.
“I totally credit him for following through on this. I might not have done anything,” says Anderson.
In October, Arbulu ordered a chest x-ray and then referred Anderson to Dr. Matt Gilman, McFarland Clinic critical care specialist and pulmonologist, for a bronchoscopy, a procedure used to view the lung. After the test, Gilman gave Anderson the bad news: She had lung cancer.
“I was healthy other than this stupid cough,” she says. “I never even remotely thought lung cancer. It was lucky that I got pneumonia because it ultimately revealed something much more serious.”
After additional tests, Anderson got some good and bad news from McFarland Clinic oncologist Dr. Venkatesh Rudrapatna. The cancer was stage 2, but was contained in Anderson’s lower left lung and hadn’t spread to lymph nodes or other organs. She’d need a lobectomy, though.
Anderson was promptly scheduled for robot-assisted surgery with Taylor.
“Dr. Taylor drew it all out for me –‘This is what we have going on and this is what we’ve got to do to get that out of you,’” says Anderson. “He told me we could do it robotically. He put me totally at ease, and I was scheduled for surgery in less than a week.”
First, however, she got a second opinion from a Des Moines oncologist, who confirmed the findings and the need for surgery, and urged Anderson to pursue the robot-assisted option.
Anderson had surgery on a Friday, spent a day in the ICCU and was home by Tuesday. Although the cancer was confined to her lung, she went through chemo treatment to ensure its eradication. Otherwise, she’s “feeling really good,” and has returned to her job as a marketing assistant at Iowa State.
“I have friends in the surgery unit and talked to them. They all had good things to say about Dr. Taylor,” she says. “We feel very comfortable with the Mary Greeley and McFarland surgical team. They’re awesome.”
A Jump on Lung Cancer
 An advanced screening program benefi ts current and former smokers.
An advanced screening program benefi ts current and former smokers.
How much damage does a smoking habit cause – even after you’ve quit? Thanks to a new test, people have a potentially lifesaving opportunity to find out.
The test is simple: a low-dose computed tomography (CT) lung scan. It can detect cancerous tumors as well as other potential lung problems.
“This is like a mammography or colonoscopy for smokers,” says Dr. Joseph Merchant, oncologist with the William R. Bliss Cancer Center, a service of Mary Greeley and McFarland Clinic. “We’re big believers in the test.”
Due to findings of a recent study, insurance covers the screening for qualified patients. To be eligible, a person must be 55 or older and have a 30-year, pack-a-day habit and no symptoms, signs or history of lung cancer. Both current smokers and smokers who have quit within the last 15 years are eligible.
“Early detection equals curable,” says McFarland Clinic surgeon Dr. Mark Taylor. “This is a signficant change in how we approach pulmonary medicine.”
Hundreds of low-dose CT lung screenings have been performed at McFarland Clinic and Mary Greeley Medical Center, resulting in several diagnoses of stage 1 lung cancer.
Biopsies can be performed if a scan indicates a tumor. For malignant tumors, there are options for patients based on the size and stage of the disease. One surgical choice is a wedge resection, which removes just a portion of a lung as opposed to an entire lobe. Taylor now performs robot-assisted lung surgery, which can result in reduced pain and faster healing for patients.
A significant clinical trial paved the way for the availability of the lung screening.
In 2002, the National Cancer Institute and the American College of Radiology Imaging Network launched the National Lung Screening Trial (NLST). “It was one of the largest and most expensive clinical trials ever conducted,” says Merchant.
The NLST trial compared two ways of detecting lung cancer: a low-dose CT scan and a standard chest x-ray. The study involved 53,454 current or former heavy smokers ages 55 to 74. Participants were randomly assigned to receive three annual screens with either option.
The group that got a CT scan had a 15 to 20 percent lower risk of death from lung cancer. The reason? Their cancer was more likely to be detected at the stage 1 level. “The result was important because no prior clinical trial had shown that we could screen for lung cancer successfully,” says Merchant.
In most cases, lung cancer patients are diagnosed at stage 3 or 4. Just 17 percent of people diagnosed with lung cancer are at stage 1.
“This means we don’t have a chance to cure them,” says Merchant. “The goal of the screening is to take people who we know are at a high risk of lung cancer and look for it at this early state. Then it is a small nodule in the lung and has not spread to lymph nodes or other organs and we can remove it before it spreads.”
The trial results, which were published in 2011, require lung screenings for qualified patients to be covered by private insurance or Medicare.
At McFarland and Mary Greeley, advanced CT technology makes the low-dose scans safer for patients who are having annual tests. No matter the findings, the screening provides another important benefit – the opportunity to scare smokers into quitting this deadly habit.
“Even if there is no cancer, they can still see the risk they are taking as we can see emphysema and scar tissue build up. We can provide counseling to help them successfully quit smoking,” says Merchant. “If they do the test once
a year, we can tell if their situation
is getting worse.”